Medical-grade Materials – The Fabric of the Future
 Over the last few years, much of the innovation in the medical device industry has been fueled by advancements in fiber and other textile technologies specifically designed for use inside the human body. These medical textile breakthroughs have supported a broad array of implantable devices ranging from vascular grafts and surgical mesh to heart valve components and orthopaedic sutures to fabric scaffolds designed to aid in tissue engineering. The fabrics these applications are built upon help deliver more life-like products with the potential to perform better, last longer, and increase comfort in the body—all of which can potentially significantly improve outcomes for patients.These advantages, along with the growing concerns around more traditional implantable materials such as metal, are causing medical device companies (MDCs) to consider textiles for more device projects than ever before. But as demand for medical textiles grows, so too does the concern about the quality of these materials and the controls implemented by the companies that process them. Many traditional materials developers and textile manufacturers, seeing a promising business opportunity, are attempting to expand into medical textile development and processing, often without the necessary medical focus or expertise.
Over the last few years, much of the innovation in the medical device industry has been fueled by advancements in fiber and other textile technologies specifically designed for use inside the human body. These medical textile breakthroughs have supported a broad array of implantable devices ranging from vascular grafts and surgical mesh to heart valve components and orthopaedic sutures to fabric scaffolds designed to aid in tissue engineering. The fabrics these applications are built upon help deliver more life-like products with the potential to perform better, last longer, and increase comfort in the body—all of which can potentially significantly improve outcomes for patients.These advantages, along with the growing concerns around more traditional implantable materials such as metal, are causing medical device companies (MDCs) to consider textiles for more device projects than ever before. But as demand for medical textiles grows, so too does the concern about the quality of these materials and the controls implemented by the companies that process them. Many traditional materials developers and textile manufacturers, seeing a promising business opportunity, are attempting to expand into medical textile development and processing, often without the necessary medical focus or expertise.
Biomedical textiles: Implantable materials
Although textile materials have been widely adopted in medical and surgical textiles for many years, new uses like biomedical implantable materials are still being found The first recorded use of fibres in medicine was mentioned in ‘Surgical Papyrus’ nearly 4.000 years ago. In the Susanta Sambita’ of the Indian Literature, written approximately 2.500 years ago. a variety of materials are mentioned including horse hair, leather strips, cotton, animal sinews and fibrous tree bark. As more research has been completed, textiles have found their way into a variety of medical applications. In addition to protective medical apparel, textiles in fibre and fabric form are used as implants, filters and surgical dressings Recent decades have witnessed major development in medical textile production, the materials they are made of the and the technology used to produce them Biomedical implants are used to aid or replace damaged tissues or organs. These materials are used in affecting repair to the body whether it is wound closure (sutures) or replacement surgery (vascular grafts, artificial ligaments, etc.)
Although the natural way to replace a defective body part would be transplantation, this is always not possible due to many reasons. Therefore, physicians use an artificial substitute (biomaterials) such as biotextiles A foreign or synthetic material or part used to replace a body part is referred to as prosthesis. Most people are familiar with artificial knees or hips. Recent reports show that 1 in 10 Americans has an implanted medical device.
The main attribute of a biomedical textile is that it should fulfill the purpose for which it was designed For example, sutures may require a biodegradable textile. An artificial ligament is permanent and is able to react more with blood cells and the surrounding tissues, compared to an external bandage which is temporary and only contacts the outer skin tissue. An implantable device should be biocompatible Biocompatibility testing evaluates the response of the host system to the medical textile. Results of this testing must be viewed along with the benefits of this device.
Requirements of an implant:
The biological requirements of a satisfactory artificial implant may be stated as follows :
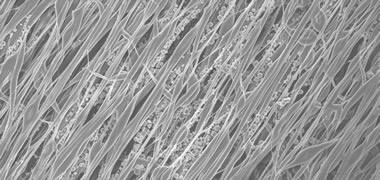
- Porosity, which determines the rate at which tissue, will grow and encapsulate the implant
- Small circular fibres are better encapsulated by human tissue than larger fibres with irregular cross-sections.
- Non-toxicity, where fibre polymer or fabrication techniques must be non-toxic and fibres should be free of contaminants.
- Biodegradability and bio-stability depending on the application A suitable artificial surface for body cells to adhere to and grow on.
Implantable biomedical textiles are a critical component in high-strength sutures and anchoring devices. They are also used as strong polymer-based cables in long bone fixation, spinal stabilization, and ligament replacement. Emerging orthobiologic applications include scaffolds and biologics containment devices. The range of possibilities is seemingly endless.
Sutures and ligatures : The term Ligature’ denotes tying something such as blood vessel or a pedicle, whereas suture’ denotes sewing by means of a needle and a thread made of suture material. Sutures are strategically located after a surgical operation primarily to hold the basic structural elements in their required sites and provide the necessary strength, retained over a period of two weeks upwards, depending on the specific site Sutures are either monofilament or multifilament threads used in surgery for wound closure. The ideal suture is a monofilament with a smooth surface that can pass through the skin without being caught and can be tightened into a single knot. The polybutylene terephthalate (PBT) suture is currently the most popular because of its acceptable strength and smooth surface. Sutures are characterized as biodegradable or non-biodegradable. Biodegradable sutures are used mainly for internal wound closures. Non-biodegradable sutures are used to close exposed wounds and are removed when the wound is sufficiently healed. These may again be of a natural or synthetic variety. The selection of the suture will depend on physical and chemical characteristics and the biological culture of the tissue in which it is placed. The absorbable natural sutures are Catgut prepared from the intestine of government inspected sheep. The great advantage of catgut is that it can be used even in the presence of infection where a non-absorbable suture cannot be used. The disadvantages of catgut are loss of tensile strength, doubted purity and cost. Collagen was invented to overcome the disadvantages of catgut The flexor tendons of beefs are converted into dispersed fibrils which are extruded and reconstituted to form collagen sutures. The absorbable synthetic sutures are Polyglycolic acid (dexon) which has the advantages of tensile strength, very little tissue reactivity, knots well. The disadvantage however is that its tensile strength falls in 15 days. Co-polymer is a suture which overcomes the disadvantage of polyglycolic acid in that its tensile strength does not fall before 4-6 weeks. The non-absorbable natural sutures are silk, waste silk, cotton, linen whereas the synthetic ones are polyamide. polyester, polyethylene, polypropylene Vicryl plus from Ethicon. is claimed to be the world’s first and only suture incorporating an antibacterial agent. It is designed to reduce bacterial colonization on the suture.
Vascular implants : The demands of the cardiovascular market have changed dramatically. The design and biomaterials used in traditional textile-based heart valves, vascular grafts, and embolic protection systems, to name a few, must now be completely redesigned from the ground up to deliver these devices by minimally invasive means. These complex devices and their associated delivery systems require an expert design partner who understands not only the mechanical challenges of catheter dimensional constraints, fatigue resistance and deliverability, but also how these differences in textile design and biomaterials influence physiological response. Having a design partner known for leadership in medical textile and fabric innovation has never been more important. Vascular graft is an artificial vein or artery used to replace segments of the natural cardiovascular system that are blocked or weakened. Grafts are implanted to bypass the blockages and restore the circulation. These are replaced in surgery to replace damaged thick arteries or veins from 6mm, 8mm or 1cm diameter. Straight or branched grafts are possible by using either the weft or warp knitting technology. Knitted vascular grafts have a porous structure, which allow the graft to be encapsulated with new tissue. The disadvantage is that this can cause hemorrhage (blood leakage) through the interstices directly after the implantation. In an attempt to reduce this nsk, knitted grafts with internal and external velour surfaces are used. Another method is to seal or percolate the graft with the patient’s blood after implantation. Porous Teflon exhibits good bio-compatibility and anticoagulant activity. However, thin blood vessels, made from Teflon tubes lead to problems. The tube consists of an inner layer of collagen, the tube itself providing strength. Research is targeted to produce artificial blood vessels of less than 3mm diameter. The main requirements are blood compatibility, porous structure, re-absorbable. easy for tissue growth and avoid clotting. Biomedical textiles and fabrics can provide important benefits to cardiovascular devices; here are just a few :
- Low Profile – Thin but durable medical textile structures can be compacted to fit within catheter-based delivery systems.
- Deliverability – Biomedical fabrics are flexible, facilitating navigation of tortuous anatomy for accurate delivery to the operative site.
- Deployment – Self-expanding Nitinol components, sheaths, and recovery/repositioning tethers are a few of the many roles medical fabrics can play in your application.
- Custom-Tailored Specifications – Whether impermeable or permeable, tapered or self-expanding, tissue incorporation or vascular filtration, biomedical textiles offer a range of possibilities to meet the exact demands of your application.
Soft tissue implants : Biomedical materials are used in applications such as soft tissue compatible artificial prostheses, artificial skin patches, artificial tendon and artificial corneas. Important properties that affect cell attachment and tissue growth are chemical structure, electnc charge, hydrophilicity, hydrophobicity, roughness of the surface, micro heterogeneity and material flexibility. Soft tissue compatible biological polymers are collagen, silk protein, cellulose, chitin and chitosan. Soft tissue artificial materials include silicone rubber, polyurethane. hydro gels and carbon fibre Silicone rubber is a cross linked polymer of poly (dimethyl siloxane). It has been used in artificial breasts, ears and noses.
Hernia repair : Meshes find use in hernia repair and abdominal wall replacement, where mechanical strength and fixation are very important Fibres can be woven or knitted into a mesh with each side designed with a specific porosity and texture to optimize its long term function. Polypropylene mesh is an example of fabrics used in hernia repair. Polypropylene is resistant to infection and is anti allergenic. Gore-Tex soft issue patch, which is used in hernia repair, is made of expanded PTFE.
Hard tissue implants : Hard tissue compatible materials must have excellent mechanical properties compatible to hard tissue Typical characteristics of polymers related to hard tissue replacements are good processability. chemical stability and bio compatibility. Applications include artificial bone, bone cement and artificial joints. Orthopedic implants are used to replace bones and joints, and fixation plates are used to stabilize fractured bones Textile structural composites are replacing metal implants for this purpose. A non-woven fibrous mat made of graphite and Teflon is used around the implant to promote tissue growth. A thorough understanding of the complicated mechanics of the rotator cuff, knee, and other joints; the delicate balance required between stabilization and motion preservation; and the stored stress/strain characteristics required for long bone fixation are critical for effective application of biomedical device designs.
Nerve guidance channel : A developing area of research is the development of nerve guidance channels that are used to bridge the damaged nerve endings and facilitate the passage of molecules secreted by the nerve and bar fibrous tissue from infiltrating the area thus preventing repair. An innovation is the use of electrically conducting polymers such as polypyrole to promote nerve regeneration by allowing a locally applied electrical stimulus. It is a blossoming field of textile research, since the nerve guidance channel may be a single continuous hollow tube, or it may be a hollow tube comprised of fibres.
Biomaterials in ophthalmology : Natural and synthetic hydro gels physically resemble the eye tissue and hence have been used in ophthalmology as soft corneal lenses Soft contact lenses are made of transparent hydro gel with high oxygen permeability. Hard contact lenses are made of poly (methyl methacrylate) and cellulose acetate butyrate Flexible contact lenses are made from silicone rubber.
Dental biomaterials : Major requirements of dental polymers include translucence or transparency, stability, good resilience and abrasion resistance, insolubility in oral fluids, non-toxicity, relatively high softening point and easy fabrication and repair. The most widely used polymer for dental use is poly (methyl methacrylate) (PMMA) and its derivatives. Other materials for denture base polymers are polysulfone and polyether polysulfone
Tissue engineering : Tissue engineenng is one of the fastest growing research fields in modern medicine. Tissue engineenng unites cell and molecular biologists, clinicians and surgeons, bioreactors and biomaterial specialists The spectrum ranges from the multiplication of simple skin cells for burnt victims to the regeneration of entire tissues and organs from the patient’s own cells Tissue engineering is the replacement of damaged tissues or organs with biologically based systems. Tissue engineering seeks to create functional substitutes for damaged tissues by combining engineering principles with those of life sciences. A small number of healthy cells are taken from a patient and allowed to multiply in the laboratory culture . These are then combined with an absorbable polymer that may be shaped to mirror the target organ or tissue. This may be fabricated in a number of ways including a three dimensional arrangement of fibres into a scaffold. The scaffold material provides structural integrity and mechanical stability in the short term. The cells are added to the scaffold and allowed to adhere and grow on the plastic material. The cell/scaffold is implanted into the patient and as the cells develop and form tissue, the plastic breaks down and is removed from the body. Thus the fundamental application of a scaffold is to grow new tissues/organs by culturing isolated cells on templates Textile structures form an important class of porous scaffolds. Embroidery technology is being widely used for medical textiles and tissue engineering. Embroideries complement the field of technology and medical textiles in a unique way since they combine very high architectural variability with the freedom of adjusting the mechanical properties in a wide range and matching it with the mechanical properties of the host tissue.
Hernia operations are among the most common surgical procedures performed, with over 20 million taking place worldwide annually. In the US alone, the associated expenditure exceeds $48 billion every year. Despite the early success of non-degradable meshes, there is still no wholly satisfactory therapy for hernia repair. In fact, non-degradable meshes are characterised by poor healing response, unfavourable foreign body reaction and in vivo erosion which lead to a failure rate of greater that 10% and a 42% incidence of recurring hernias. Recurring hernias cause further distress to patients, compromising their quality of life, all the while putting an additional financial strain on healthcare systems.
Researchers at NUI Galway – one of Ireland’s foremost centres of academic excellence – are leading a European project to develop a new product for use in hernia operations. The Network of Excellence for Functional Biomaterials (NFB)-led consortium has been awarded an EU-FP7 grant worth € 2.7 million for a proposal entitled Targeting Hernia Operation Using Sustainable Resources and Green Nanotechnologies. The overall objective of the Green Nano Mesh research project is to develop a novel mesh for use in hernia operations.
Summary
Textiles are developing into interdisciplinary high tech products with interesting chances on the market. Owing to the greater co-ordination among textile technologists and medical researchers, textile products for surgical procedures are being developed indigenously. Textile structures in implantation are identified by structure, material composition, behavior of fibre surface and degradation. Developments of biologically friendly and predictable absorbable fibres will be of great interest, both as suture materials and as the basis of tissue engineering constructs. Improved absorbable fibres will be of great interest, both as suture materials and as the basis of tissue engineering constructs. Improved absorbable fibres will be necessary as new sterilization technologies are introduced to meet evolving environmental specifications. Advances in textile technology will clearly bring a new and improved group of biomedical textiles.